Minimally Invasive Spine Technologies
In the past decade Spine surgery has witnessed exponential growth in techniques and technologies. Numerous patients have benefited so far with spinal surgery. With growing experience and periods of follow-up after conventional spine surgeries, surgeons started to face the flip side of these conventional open surgeries. Conventional surgeries have yielded results in many patients but have also left many patients with dissatisfaction.
Origin of Concept of Minimally Invasive Spine Surgery
Conventional spinal surgery aims at thorough decompression, rigid stabilization and fusion. These objectives are achieved with large incisions, extensive soft tissue dissection, laminectomy etc. These approaches lead to a plethora of untoward effects like…
- Larger blood loss during surgery
- Delayed post-operative recuperation
- Increased hospital stay
- Delayed return to functional status
- Extensive scar tissue formation at operated area and into the epidural space. ( which may cause neural compression )
All these have given rise to a very large group of patients termed as “FAILED BACKs “. Not only do these failed back patients cast a shadow on spinal surgeries but it is not easy to revise these surgeries and produce excellent results.
This forced the spinal surgical community to switch from physiologically devastating conventional surgery to a friendlier and less invasive surgical technique called “Minimally Invasive Spine Surgery”
Concept of Minimally Invasive Spine Surgery
MISS is developed with a concept to make surgery as near physiological as possible. The aims are
- Preserve as much normal tissue as possible
- Eradicate the pathology with least possible damage to normal biomechanical physiology.
- Improve and expedite the post-operative rehabilitation
- Reduce the occurrence of some of the untoward effects of conventional open surgeries like fibrosis and scarring that may cause nerve compression.
In a nutshell, MISS aims to help a patient to get back to his normal active life with the least possible surgical intervention.
Minimally Invasive Spine Surgery (MISS)
Approaching the Spine
- Instead of extensive soft tissue dissection the MISS approach aims to dilate the muscle avoiding cutting and stripping the muscles from the lamina and spinous process.
- It preserves the spinous process and lamina as much as possible, maintaining the natural barrier to fibrous tissue in-growth.
- Facet and facet joint capsule are spared completely to prevent iatrogenic instability of motion segment.
- For the anterior approach, Mini-Thoracotomy and Mini-open retroperitoneal approaches have been employed to reduce postoperative approach related morbidity.
Minimally Invasive Disc surgeries
For many years laminectomy and discectomy have been replaced by microdiscectomies for cervical and lumbar disc herniations in a stable motion segment. However, microdiscectomy requires epidural dissection, coagulation of epidural blood vessels, nerve retraction, minimal muscle stripping and ligamentum flavum resection.
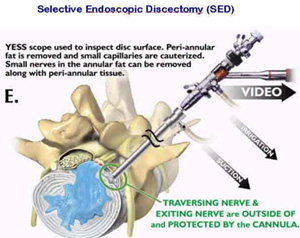
To avoid all the above surgical violations of normal tissue, discectomies are now done via an endoscopic approach. PELD (percutaneous endoscopic lumbar discectomy)/ PECD (percutaneous endoscopic cervical discectomies) are done through a posterolateral transforaminal approach for lumbar spine and anterior approach for cervical spine. They are done under local anesthesia avoiding the morbidity and risks associated with general anesthesia. To approach the Kambin’s Safe Zone in the transforaminal approach, muscles are dilated upto just 8mm.
There is negligible surgical violation of the epidural space around the spinal nerves. The patient can walkout of the operating room. The surgery is done on a day care basis.
Motion Preservation surgeries
Fusion surgeries have been the gold standard surgical technique for the unstable spine and for multiple degenerated disc disease. Fusion has its own disadvantages like extensive surgical dissection, blood loss, possibility of pseudo-arthrosis and adjacent segment disease. To avoid these complications, MISS attempts to preserve the mobility of a motion- egment. This is done either by using a total cervical/lumbar disc replacement or by using the posterior interspinous stabilizing devices. Cervical disc replacement has already proven itself in yielding benefits to patients as compared to ACDF (anterior cervical discectomy and fusion). Lumbar disc replacement is still in its very early stage and we need to wait till it really proves itself.
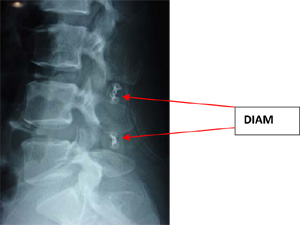 Inter-spinous devices work by restoring the posterior tension band of a motionsegment, have already been successful in degenerated motion-segment. There are a number of inter-spinous devices available like X-Stop, DIAM, Coflex, Wallis etc. They are useful to offload the degenerated disc, to widen the foramen by keeping the segment in slight flexion, to off-load the facets by being a load- haring device biomechanically while at the same time providing a restricted safe motion to a segment.
Inter-spinous devices work by restoring the posterior tension band of a motionsegment, have already been successful in degenerated motion-segment. There are a number of inter-spinous devices available like X-Stop, DIAM, Coflex, Wallis etc. They are useful to offload the degenerated disc, to widen the foramen by keeping the segment in slight flexion, to off-load the facets by being a load- haring device biomechanically while at the same time providing a restricted safe motion to a segment.
Minimally Invasive Fusion Surgeries
 There are multiple pathologies of the spine that can only be treated by a rigid stabilization and fusion like spinal trauma, lytic or dysplastic lysthesis, infection, tumor, etc. When fusion is the only option, minimally invasive fusion is the bridge that least can avoid approach related deleterious effects on a human spine.
There are multiple pathologies of the spine that can only be treated by a rigid stabilization and fusion like spinal trauma, lytic or dysplastic lysthesis, infection, tumor, etc. When fusion is the only option, minimally invasive fusion is the bridge that least can avoid approach related deleterious effects on a human spine.
In Minimally Invasive fusion surgeries, the spine is approached with a muscle friendly approach as described. Instead of doing a wide decompression, micro-decompression is attempted to preserve the natural barrier. Instead of opening very widely for pedicle screw insertion, the screws are placed percutaneously from separate stab incisions. Screws are connected with a rod that is also inserted percutaneously. This technique not only preserves a healthy muscle cover but also reduces the blood loss during surgery making patients recover faster.

Minimally Invasive Surgery for Fractures of Spine
Most spinal fractures require decompression and stabilization by anterior and/or posterior approach. Posterior stabilization now can be achieved by using percutaneous screws. With percutaneous screws, posterior stabilization can be achieved through a stab incision without any damage to soft tissue or without significant blood loss.
In cases of compression fractures which be traumatic, osteoporotic or pathological in origin, surgeons now perform either vertebroplasty or balloon kyphoplasty keeping a minimally invasive concept in mind. Balloon kyphoplasty has some advantages over more commonly performed vertebroplasty. By using Balloon kyphoplasty we can restore the height of compressed vertebra to an extent. Kypoplasty reduces the chances of cement leak and also reduces the incidence of adjacent level fracture post procedure.

Advantages of MISS
- Less tissue trauma
- Less blood loss
- Preservation of physiologically important normal structures
- Rapid postoperative recuperation
- Decreased hospital stay
- Early return to normal functional status
- Decreased incidence of failed back surgeries
- Increased patient satisfaction
Conclusion
Minimally invasive spinal surgery is in its infancy. With further advances in optics and surgical technologies even more spinal pathologies can be treated with the MIS concept thereby increasing patients’ satisfaction and also the success rate of spinal surgeries. MISS done so far has immensely benefited patients and has reduced some of the untoward effects of conventional open surgery.

No Comments